Study: Treat 5% of Hepatitis C patients with new drugs to reduce infections, costs
Researchers at USC Schaeffer Center for Health Policy & Economics and other institutions found the health care system would save more lives and money than the current approach if more patients were treated with the newest drugs earlier in the disease’s progression.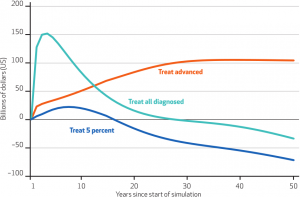
Contact: Emily Gersema, (213) 740-0252 or gersema@usc.edu
Treating 5 percent of all hepatitis C patients with the latest drugs would be more effective at reducing infections and health care costs than the current approach, a new study shows.
The cost-benefits analysis by researchers from the USC Schaeffer Center for Health Policy and Economics and other institutions compares three treatment options to the current approach, or “baseline” scenario, which treats patients in the most advanced stages of the disease when they may need a costly liver transplant.
“We made a mistake with HIV by limiting access to treatment to just people who had AIDS, and we ended up with a virus that has been with us for decades,” said corresponding author Dana Goldman, who is the Schaeffer Center director, and a professor at the USC School of Pharmacy and the Price School of Public Policy. “We didn’t initially treat HIV aggressively enough in part because the science wasn’t there to justify it. With hepatitis C, we have the science. We just need to find a way to finance it.”
The researchers found that a “treat 5 percent” approach would reduce infections from 2.7 million to 39,000 cases in 50 years, compared with the current approach, relying on older drugs, which would reduce infections to 207,000 cases in 50 years. Under the “treat 5 percent” scenario, health care expenditures would drop below the baseline’s costs within 20 years of implementation.
The researchers said that although treating all patients is the best option for reducing infections in 50 years to 1,400 cases, it is unrealistic, given the limits of health care funding.
The study, to be published on Oct. 5 in the journal Health Affairs, is believed to be the first analysis to account for how the disease progresses in a patient and the ways in which it can spread.
It also differs from prior analyses in that it accounts for “social value” — the benefits of treatment for the patient and society, as well as drug manufacturer profits. Patient benefits include what researchers labeled as “Quality-Adjusted Life-Years” for patients. One QALY represents each year that a drug enabled a person to have perfect health, or it is equal to every two years that a drug enabled a person to live half as healthy.
Treatment scenarios
• Treat all: Using the latest drugs, this approach would have the greatest social value, generating up to $1.2 billion in QALYs and saving up to $139 billion in medical costs over a 50-year span. Cases would drop to 1,400 in 50 years.
• Treat advanced: This is the most expensive option and, using the latest drug treatments, would cost nearly $100 billion per year after nearly 25 years of implementation. Cases would drop to 103,000 patients in 50 years. This approach also generates the lowest social value — up to $175 billion in QALYs.
• Treat 5 percent: The cheapest option is to treat 5 percent of all patients, regardless of the disease’s acuity. Net expenditures spike to $22 billion by the eighth year of this scenario but then sink below the cost of the current treatment approach by year 20. The social value could reach up to $437 billion in QALYs.
U.S. infections
Goldman said a common misconception is that hepatitis C patients are drug users when in fact most are baby boomers who were infected via blood transfusions or unsterile medical equipment before 1992.
Hepatitis C also is transmitted two other ways. One is by HIV-infected men through sex. The other is intravenous drug use. With heroin use on the rise nationwide, some health officials anticipate a second wave of infections.
The disease can remain latent for up to 15 years and then worsen, causing in some cases cirrhosis or death. Five patients per every 100,000 cases die annually in the United States, federal health statistics show.
“The important point is that when you treat hepatitis C, you benefit not only that person but also everyone they might infect,” Goldman said.
Imposing drug price controls on costly hepatitis C drugs may sound like a simple solution to make them more accessible and affordable, but Goldman warned that could backfire and stifle research and development for all disease treatments.
The study’s lead author was Karen Van Nuys, a senior research economist at Precision Health Economics. Other contributors were Ronald Brookmeyer of UCLA; Jacquelyn W. Chou of Precision Health Economics; David Dreyfus of Arete Analytics; and Douglas Dieterich of the Icahn School of Medicine at Mount Sinai.
Precision Health Economics was founded by three health policy and economics experts, including Goldman, who is chairman of the firm’s Value and Evidence Advisory Board, and its executive economist.
The study was funded by Gilead Sciences, a pharmaceutical company that makes Sovaldi and Harvoni treatments for hepatitis C.
# # #
